Back pain

Back pain is a common symptom that affects 60–80% of people at some time in their lives. The prognosis (outcome) is generally good. After 2 days, 30% are better and 90% have recovered by 6 weeks. Recurrences of pain may occur and about 10–15% of patients go on to develop chronic back pain that may be difficult to treat. Psychological elements, such as job […]
Haemorrhoids (piles)
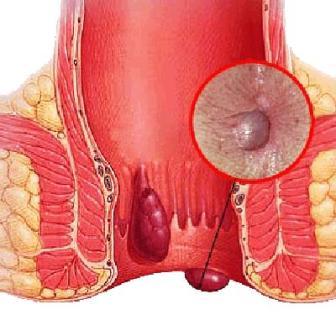
Haemorrhoids, also known as piles, are swellings containing enlarged blood vessels found inside or around the bottom (the rectum and anus). When symptoms do occur, they may include: bleeding after passing a stool – the blood is usually bright red itchy bottom a lump hanging down outside of the anus, which may need to be pushed […]
Wrinkles

Wrinkles, a natural part of aging, are most prominent on sun-exposed skin, such as the face, neck, hands and forearms. Symptoms Wrinkles are the lines and creases that form in your skin. Some wrinkles can become deep crevices or furrows and may be especially noticeable around your eyes, mouth and neck. When to see a […]
Whooping Cough

Whooping cough (pertussis) is a highly contagious respiratory tract infection. In many people, it’s marked by a severe hacking cough followed by a high-pitched intake of breath that sounds like “whoop.” Symptoms Once you become infected with whooping cough, it takes about seven to 10 days for signs and symptoms to appear, though it can […]
