Back pain

Back pain is a common symptom that affects 60–80% of people at some time in their lives. The prognosis (outcome) is generally good. After 2 days, 30% are better and 90% have recovered by 6 weeks. Recurrences of pain may occur and about 10–15% of patients go on to develop chronic back pain that may be difficult to treat. Psychological elements, such as job […]
Haemorrhoids (piles)
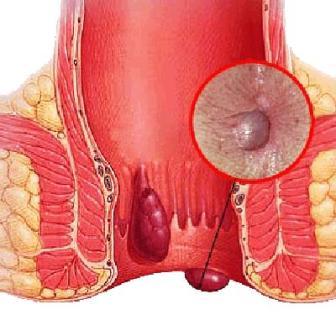
Haemorrhoids, also known as piles, are swellings containing enlarged blood vessels found inside or around the bottom (the rectum and anus). When symptoms do occur, they may include: bleeding after passing a stool – the blood is usually bright red itchy bottom a lump hanging down outside of the anus, which may need to be pushed […]
Prenatal Care

Prenatal care helps decrease risks during pregnancy and increase the chance of a safe and healthy delivery for the mother and child. Regular prenatal visits can help your doctor monitor your pregnancy and identify any problems or complications before they become serious. Prenatal care ideally starts at least three months before you begin trying to […]
Pre Conceptional Care

What is preconceptional care and why is it important? Having a healthy pregnancy is one of the best ways to promote a healthy birth. Getting early and regular preconceptional care improves the chances of a healthy pregnancy. This care can begin even before pregnancy with a preconception care visit to a health care provider. Preconception […]
Postnatal Care

The postnatal period lasts six to eight weeks, beginning right after the baby is born. During this period, the mother goes through many physical and emotional changes while learning to care for her newborn. Postnatal care involves getting proper rest, nutrition, and vaginal care. Getting Enough Rest Rest is crucial to new mothers who need […]
Ovarian Cancer
Ovarian cancer is a type of cancer that begins in the ovaries. Women have two ovaries, one on each side of the uterus. The ovaries — each about the size of an almond — produce eggs (ova) as well as the hormones estrogen and progesterone. Ovarian cancer often goes undetected until it has spread within […]
Natural Family Planning
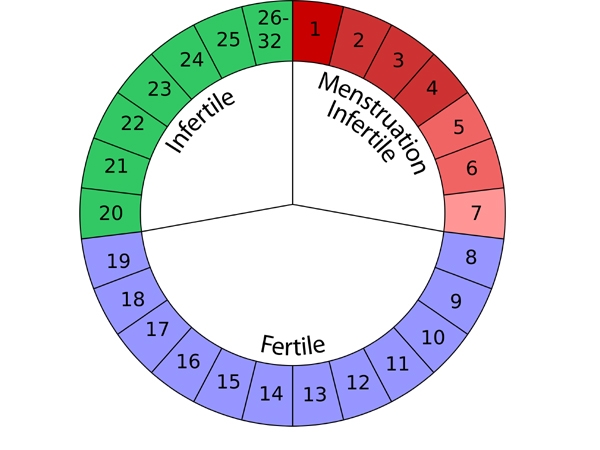
What is natural family planning? Natural family planning is a method of preventing pregnancy, without using pills or devices. It is based on being able to predict your fertile time. This is the time you are likely to conceive. Pregnancy is avoided if you don’t have sex during this fertile time or use other methods […]
Miscarriage

A miscarriage is the loss of a baby before the 20th week of pregnancy. More than 80% of miscarriages occur within the first three months of pregnancy. They are less likely to occur after 20 weeks’ gestation; if they do, they are called late miscarriages. What Are the Symptoms of Miscarriage? Symptoms of a miscarriage […]
Menstrual Problem

What Are Menstrual Problems? Menstrual cycles often bring about a wide array of uncomfortable symptoms leading up to your period. Premenstrual syndrome (PMS) encompasses the most common issues, such as mild cramping and fatigue, but the symptoms usually go away when your period begins. However, other, more serious menstrual problems may also arise. Menstruation that […]
Menopause

Menopause is defined as occurring 12 months after your last menstrual period and marks the end of menstrual cycles. Menopause can happen in your 40s or 50s. Menopause is a natural biological process. Although it also ends fertility, you can stay healthy, vital and sexual. Some women feel relieved because they no longer need to […]
